Posted on: 12/July/2025 | By Dr. Ritesh Gaikwad
“Young Man, Old Problem”: A New Approach to Recurrent Varicose Ulcer Using IVUS-Guided Iliac Vein Stenting
Chronic venous insufficiency in young adults is often underestimated or incorrectly attributed to superficial vein disease. Yet, for many patients, especially those with recurrent symptoms despite previous interventions, the real pathology lies deeper. This case highlights how a young patient with a seemingly routine venous ulcer revealed a much more complex underlying problem — one that could only be effectively managed using intravascular ultrasound (IVUS) and iliac vein stenting.
Introduction: A Familiar Story with an Unfamiliar Ending
Chronic leg ulcers in younger patients are uncommon but not unheard of. However, what’s more unusual is when these ulcers persist or recur despite repeated superficial vein interventions. This is where the story of a 26-year-old man becomes a lesson in looking beyond the obvious.
The patient, a young male with a 4-year history of varicose veins, had undergone two sessions of endovenous laser ablation (EVLA) on both limbs and even an open surgical procedure on the right side. Despite all this, he continued to suffer from swelling, pain, and eventually a non-healing ulcer that brought him limping into our vascular surgery department.
The initial clinical suspicion was straightforward — recurrent superficial venous insufficiency. But the persistence and severity of symptoms, especially the ulceration, hinted at a more proximal cause that had likely been missed in previous assessments.
Reassessing the Problem: The Role of Proximal Venous Outflow Obstruction
A thorough clinical examination revealed classic signs of chronic venous insufficiency — edema, varicosities, and a painful medial leg ulcer. However, the pattern and chronicity of his symptoms suggested an underlying outflow obstruction, particularly in the iliac veins, which often remains undiagnosed in such cases.
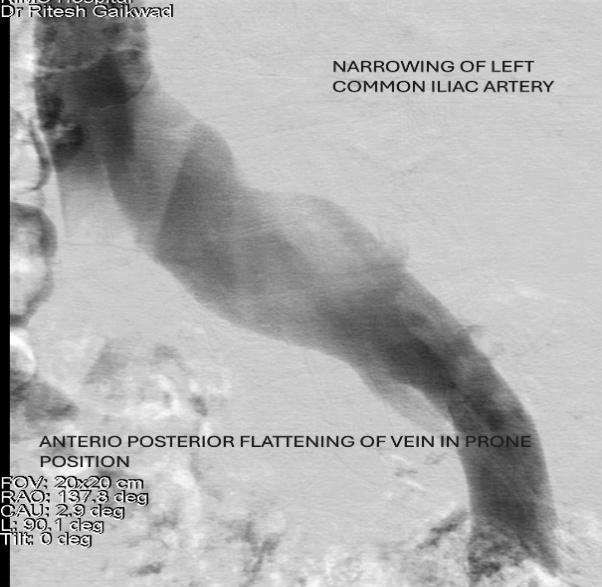
Initial non invasive test ( physiological testing) like venous reflux time and MVO/ SVC ratio and imaging with an MR venogram suggested iliac vein compression. However, MR and CT venography, although useful for screening, often fall short in evaluating iliac vein pathology due to the collapsible, thin-walled nature of veins. In this case, the imaging showed a “pancaking” of the iliac vein — a classic feature of May-Thurner syndrome (left iliac vein compressed by the overlying right iliac artery and spine) or non thrombotic iliac vein lesion (NIVL).
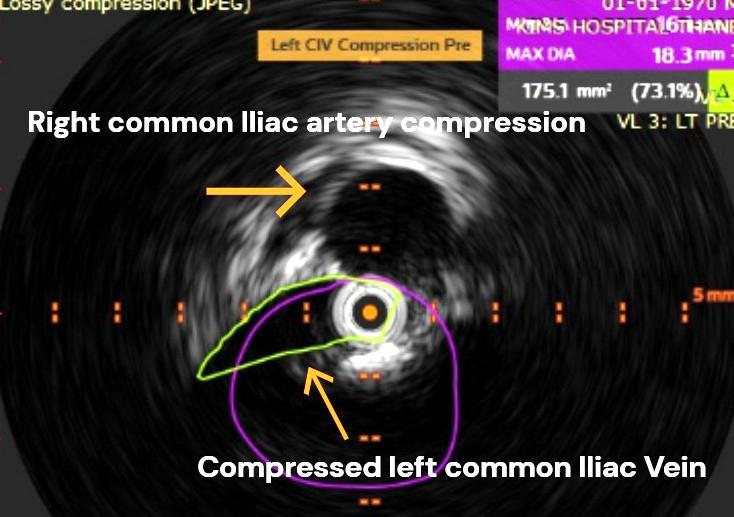
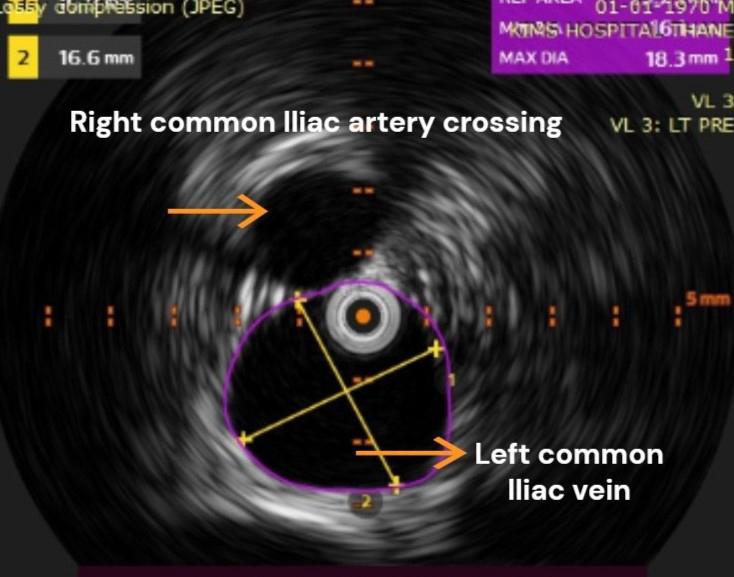
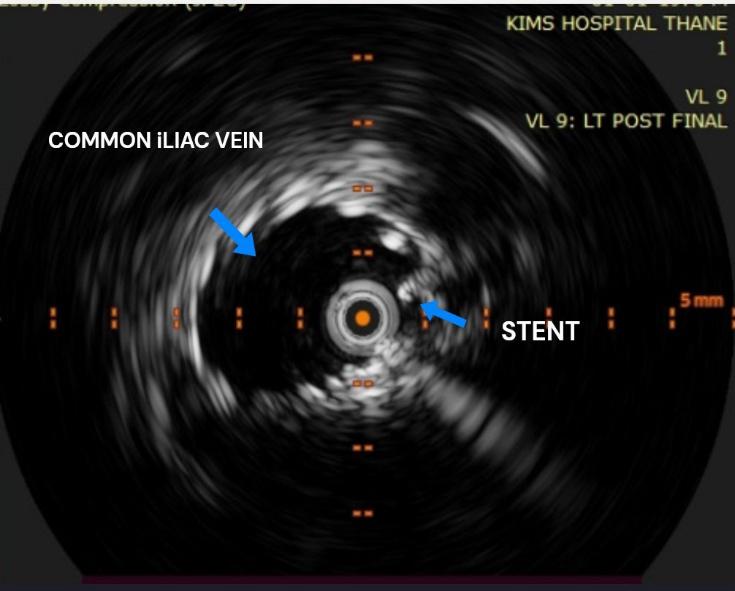
But as we know, conventional imaging provides only indirect clues. What we needed was a definitive, real-time, intraluminal view of the vein — and for this, IVUS proved indispensable.
IVUS: A Game-Changer in Venous Diagnostics
Intravascular ultrasound (IVUS) allows direct visualisation of the vessel lumen, wall, and surrounding structures. Unlike venograms, which rely on contrast filling and can miss non-occlusive lesions, IVUS gives real-time, high-resolution images that can quantify compression, determine cross-sectional area, and guide precise stent sizing and placement.
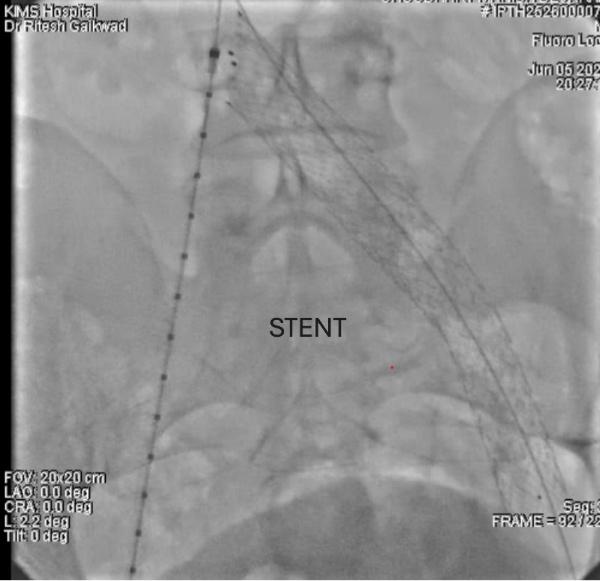
We performed IVUS in both prone and supine positions, revealing significant extrinsic compression of the left iliac vein. The degree of narrowing was clearly underestimated on MR venography, reaffirming the superiority of IVUS in such cases. With this definitive diagnosis in hand, we proceeded to intervene.
Treatment: Simple, Safe, and Swift
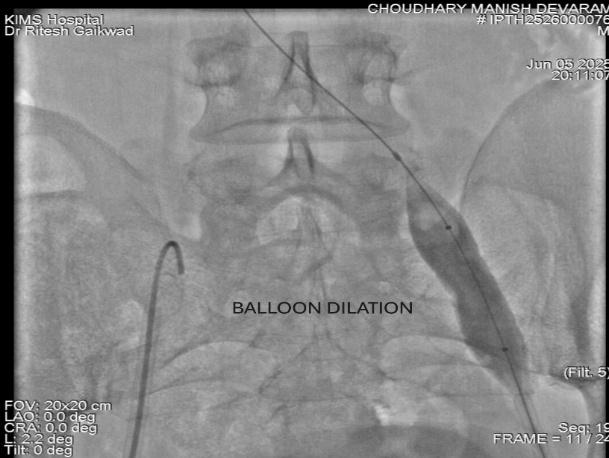
The patient underwent balloon angioplasty followed by deployment of a dedicated self-expanding venous stent in the compressed segment of the left iliac vein. The procedure was uneventful, completed in under an hour, and the patient was mobilized within two hours postoperatively.
The immediate postoperative period was remarkable. By the next day, he reported over 90% reduction in swelling and pain. Patient was discharged with rapid wound healing already underway — a dramatic turnaround after years of ineffective treatment.
Lessons Learned: Why Deep Veins Matter
This case underscores a crucial point — young patients with recurrent varicose veins and leg ulcers may have a proximal venous outflow obstruction that is often overlooked by physician and treating physician. Traditional focus on superficial veins alone can result in years of futile interventions and chronic disability.
In such scenarios, failing to consider iliac vein compression — often seen in variants of May-Thurner syndrome and NIVL — can delay definitive treatment. Even when suspected, conventional imaging may not detect it reliably. This is where IVUS becomes a critical diagnostic and therapeutic tool.
More importantly, treating the root cause with iliac vein stenting, particularly using modern, dedicated venous stents, offers excellent results. These stents are designed to handle the dynamic, compressive environment of the pelvis and provide long-term patency with minimal complications.
Broader Implications for Vascular Practice
As endovenous interventions for varicose veins become increasingly common, we must remain vigilant for underlying pathologies when patients present with recurrence or poor response to treatment. Chronic venous ulceration in a young adult should never be taken lightly or assumed to be merely a failure of superficial ablation.
Instead, we need a shift in our diagnostic algorithm — one that routinely includes evaluation of the iliocaval venous system, especially in refractory cases. The cost and expertise required for IVUS may be higher, but so is the value it brings in clarity of diagnosis and precision of therapy.
Furthermore, with the increasing availability of modern venous stents and minimally invasive tools, we can now offer solutions that were previously unimaginable for such patients. The key is in recognizing the problem early and not stopping at the superficial layer — quite literally.
Conclusion: Looking Beneath the Surface
This case reminds us that good outcomes in vascular surgery often depend not just on what we see, but on where we look. For this young man, years of pain and disability were resolved not by repeating previous treatments but by revaluating the diagnosis and treating the true cause: outflow obstruction.
IVUS-guided venous stenting is more than just a technical advancement — it’s a paradigm shift. And for patients like this, it means the difference between chronic suffering and rapid, lasting relief.
Let this be a reminder that even in the young, old venous problems can hide in plain sight — and that a deeper look can bring lasting healing.
Dr. Ritesh Gaikwad
MBBS, DNB General surgery and DNB (Vascular Surgery)
Consultant Vascular & Endovascular Surgeon
KIMS Hospitals